A question I hear all the time is this: Is adrenal fatigue real or not?
After writing a guest post for Jen Sinkler, I was somewhat embroiled in a heated discussion about whether or not “adrenal fatigue” really exists.
The argument from the most reasonable critic was this:
Adrenal fatigue is not a real condition. We need to stop perpetuating this term. Here is the problem: You’re tired and someone says you have adrenal fatigue. You take one of those bull— salivary diurnal cortisol tests that you ordered online. You get the results and it says you have adrenal fatigue. OR someone just diagnoses you with adrenal fatigue. All of a sudden you possibly missed a potential real diagnosis (anemia, hypothyroidism, sleep apnea, etc) and you just labeled it with a made of up diagnosis. This is super dangerous and why we cannot go around discussing fake diseases.
I understand what this critic is saying, and to an extent I agree with it. If people are being diagnosed with “adrenal fatigue” when they actually have something more insidious going on, they’ll be in trouble if all they do is take a saliva test, change their diet and lifestyle, and take a handful of supplements.
However, the majority (if not all) of my “adrenal fatigue” clients have already gone to their doctor for help, and after rigorous but inconclusive/negative testing are told “you’re fine” and are often prescribed an antidepressant or Ambien.
The short answer to the question in my headline? No.
“Adrenal fatigue” is not a real diagnosis. But I strongly believe that the condition the term is describing is very much real.
What is Adrenal Fatigue, anyway?
“Adrenal fatigue” is a misnomer – a colloquial term for HPA Axis Dysregulation, which itself is not a “clinical diagnosis” (yet) but certainly exists in the literature and is associated with chronic stressors like overtraining, PTSD, and sleep disruption.
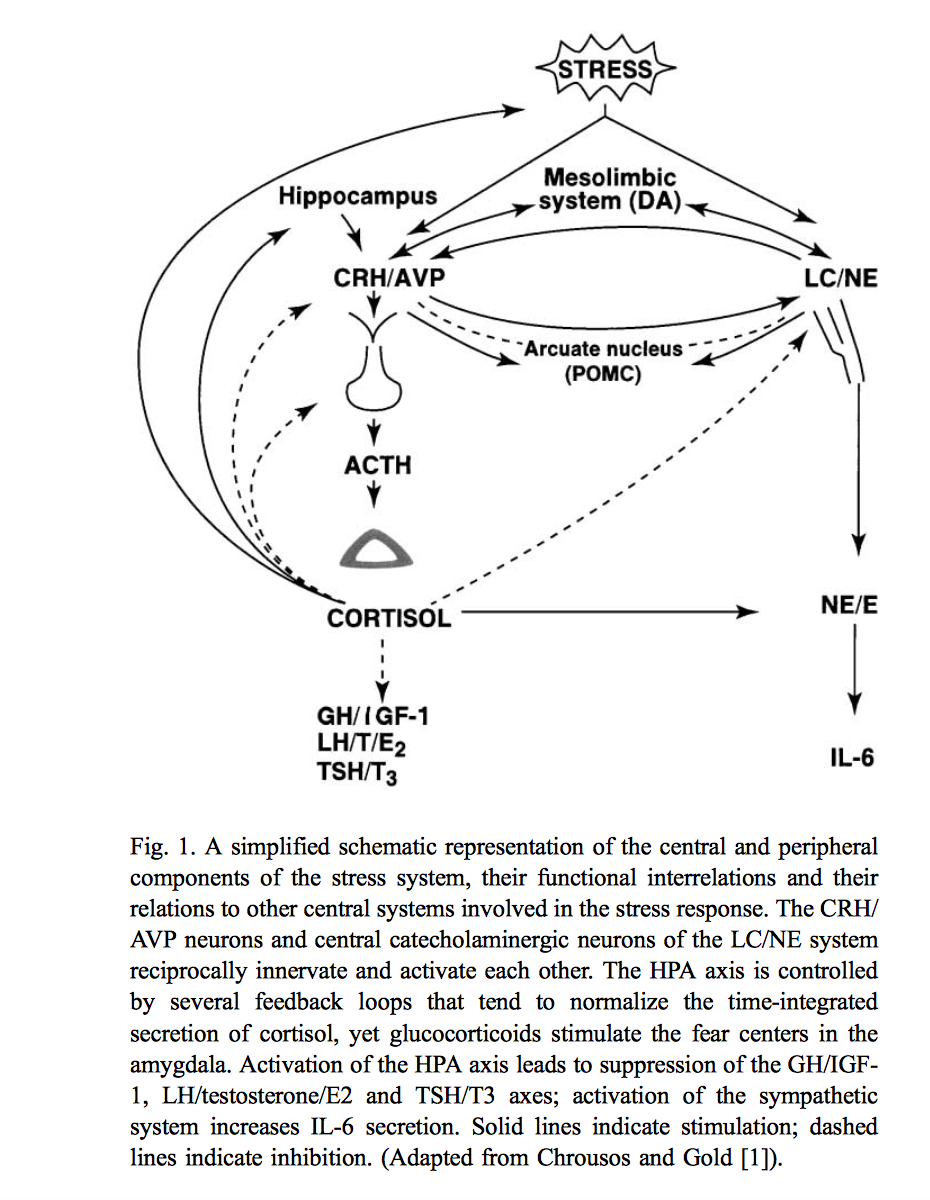
The hypothalamic-pituitary-adrenal axis (HPA axis) is the control center for your body’s stress response. When you get stressed, the concentrations of your HPA axis hormones are increased. The hypothalamus releases corticotropin-releasing hormone (CRH), which is the first of a cascade of hormonal changes that eventually result in the production of cortisol (the “stress hormone”) from the adrenal glands. Elevated cortisol levels direct the distribution of energy to different organs that underlie the stress response, such as the brain, heart, and muscles. This is a normal response and is something your body was designed to do.
As you can see in the diagram above, the HPA axis has several feedback loops that allow the body to normalize the production of stress hormones such as cortisol.
This prevents your body from becoming overstimulated by a source of stress that is more chronic in nature. This process is called “habituation”, where the body is able to decrease its physiological activation to certain stressors. (1) You might also call this adaptation. It’s normal and healthy, and prevents the negative side effects of chronic HPA activation.
However, certain people are unable to properly habituate to the daily stress they face, particularly if the stress is much more significant than simply a traffic jam on the way to work. Think of stressors like an abusive relationship, a sick family member, or serious financial strain. (I’d consider chronic malnourishment or overtraining at this same level from a physical stress perspective.)

What happens when the HPA Axis gets dysfunctional?
When the HPA axis is no longer able to adapt to daily stressors appropriately, this is when the symptoms of “adrenal fatigue” become an issue.
The typical pattern of adrenal dysfunction is a high level of cortisol to start, then a drop to low cortisol, though some stressful events are traumatic enough to send the HPA axis straight into low cortisol output. Some people also experience a reversal of the circadian rhythm of cortisol output, where their cortisol is low in the morning and high in the evening.
The adrenals don’t get “fatigued” – they eventually produce less cortisol over time as the hypothalamus stops stimulating them appropriately. (Fun fact: This is why many people say “adrenal fatigue” doesn’t exist. Because the name sucks.)
Any level of cortisol disturbance due to chronic HPA axis activation falls into the umbrella term of “adrenal fatigue”. Failure of the HPA axis to respond appropriately to acute stress is another cause of symptoms. Those with HPA axis dysregulation typically have developed a new “normal” of steady state low or high cortisol, and depending on which state they fall into, different symptoms can emerge.
These symptoms can include:
- Weight gain or loss
- Frequent illness (e.g. colds, flus)
- Reduced sex drive
- Lightheadedness
- Poor memory
- Fatigue, lethargy and exhaustion
- Insomnia
- Coffee addiction
- Salt, sugar, and fatty food cravings
- Worsened PMS
- Pain in the upper back or neck
- Mild depression
- Food allergies
- Dry and thin skin
- Hypoglycemia
- Low body temperature
- Nervousness and anxiety
- Heart Palpitations
- Unexplained hair loss
- Alternating constipation and diarrhea
- Heartburn or dyspepsia
One argument from adrenal fatigue critics is that the symptoms list is too diverse and could be related to any number of diagnosable conditions. While this is true, that doesn’t invalidate the fact that chronic HPA axis activation and subsequent dysfunction can cause those symptoms in many individuals as well. These may seem like highly variable, nonspecific symptoms, but that doesn’t mean they’re not primarily due to stress.
In scientific literature, failure of the HPA axis to habituate to chronic stress is associated with a wide range of physical and mental health outcomes, including exhaustion, depression, anxiety, low self esteem, and central fat accumulation (2, 3, 4) Low steady state cortisol is often seen in both PTSD and chronic fatigue syndrome (CFS). (5, 6)
What’s worse, HPA axis dysfunction can affect the regulation of immune and inflammatory processes, which can influence the risk of infectious disease, autoimmunity, heart disease, and even some cancers. (7)
Your ability to respond and adapt appropriately to stress will significantly affect how your body responds to chronic stressors over time. If your body stops responding appropriately, your risk of these conditions rises substantially.

Why do some people react to stress worse than others?
It’s important to realize that not everyone responds and adapts to similar stressors the same way. For example, research shows that people who are prone to “rumination” (i.e. overthinking and focusing on past stressors) have a reduced ability to adapt to repeated stress. (8) Just one night of sleep deprivation has been shown to impact the body’s ability to adapt to stress as well. (9)
This would indicate that certain personality types and/or lifestyle factors may put someone at higher risk for HPA axis dysregulation. And it would explain why certain people seem to be fine when exposed to regular intense stress (professional athletes, military personnel, etc.) while others develop HPA axis dysfunction from seemingly “normal” stress (e.g. doing Crossfit 5 days a week while eating a low calorie diet and sleeping 6 hours a night.)
For those of you suffering from adrenal fatigue syndrome, I’m sure this resonates with you deeply.
Would you like to save this post?
Your email address is 100% safe and will never be sent spam.
Why is it that you can eat a “healthy” diet and exercise regularly, but have crushing fatigue, while your friends or family might eat junk and sit around all day and feel completely fine?
All of us have different levels of response to the same stressors and a lifestyle that might cause HPA axis dysfunction in you might be completely manageable for a friend. That’s why individualization is key when recovering from HPA axis related disorders.
So, is adrenal fatigue “real”?
As you can see, “adrenal fatigue” is not a recognized medical diagnosis, and the term is misrepresenting the processes happening in your body when you are unable to adapt to chronic stress.
However, that doesn’t mean the condition isn’t real.
HPA axis dysregulation is very much a real condition, and it’s important to recognize the importance of healthy lifestyle changes to reduce or eliminate the symptoms associated with chronic HPA axis dysregulation.
If you’ve been to the doctor for any of the symptoms I listed above, gone through multiple diagnostic tests, and have found nothing, you need to take a closer look at your diet and lifestyle and identify if you’re engaging in behaviors that are causing your body to be under constant stress.
This is an extremely common issue in the Paleo community, particularly for women. I see it all the time with my one-on-one clients – people eating way too little for the amount of exercise their doing, and experiencing severe hormonal disturbances from the HPA axis disruption.
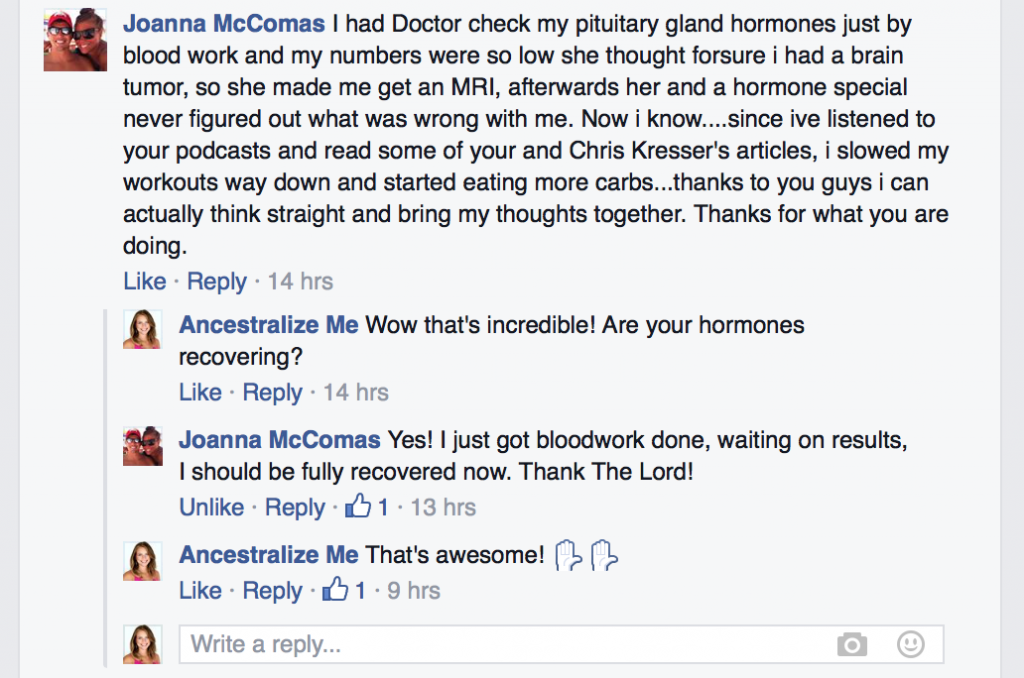
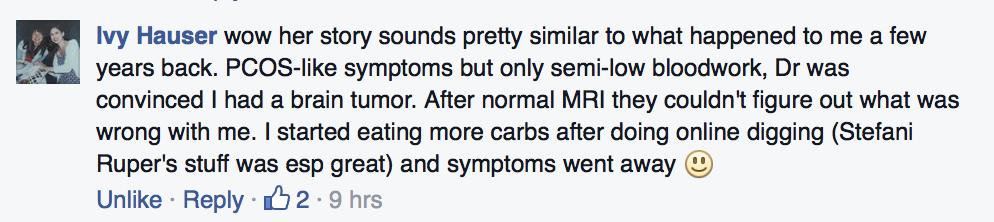
Just look at the experiences Joanna and Ivy had:
It frustrates me that there are so many people out there who are harming their HPA axis function in the pursuit of better health and fitness, and when they finally see their doctors about the symptoms, most docs don’t think to look at the person’s diet and lifestyle as a potential cause.
Why did we create Paleo Rehab: Adrenal Fatigue?
Both Kelsey (my business partner) and I have struggled with hormonal issues related to stress, including low cortisol, and that’s why we’re passionate about helping people who are in a similar condition.
In no way would we ever consider what we’re doing “diagnosing and treating” anything. We’re just trying to help people who are driving themselves into the ground with restrictive dieting, overexercising, high levels of stress, and poor sleep.
The reason we created the program is because we had so many clients coming to us on these restrictive diets and 8 million supplements, and the biggest issue was their inadequate diet and overly stressful lifestyle. So we figured we’d create a program to teach the basics to a wider audience.
Most of our students are the ones who went to their doctor(s) for help and were told that there was “nothing wrong with them”. Sure, from a medical perspective there may be nothing treatable, but from a lifestyle perspective there is a huge room for improvement, especially in the psychological part that many of our clients struggle with most prominently.
Ultimately our ideal client is the person with disputed HPA axis function due to their high stress diet and lifestyle choices, and we help them address those basic issues in detail.
For those critics saying that Kelsey and I are using a “made up term” to dupe people into buying a bogus program, I have two things to say. First of all, we’re helping people address HPA axis dysfunction in the program, and if you want to call it that instead, by all means – do it.
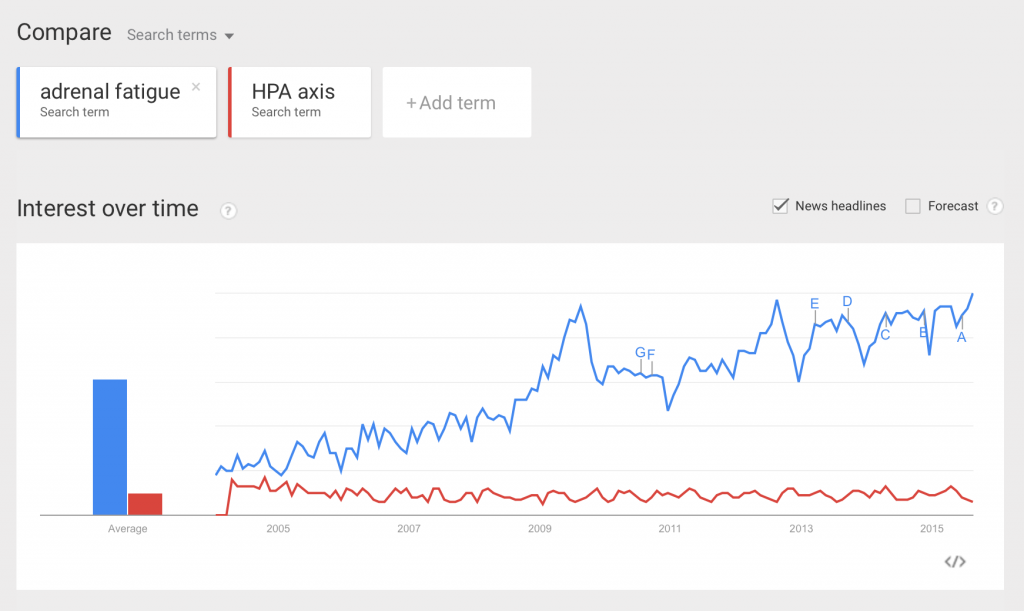
But that leads me to my second point: had we called the program “Healing from HPA Axis Dysregulation”, I can guarantee NO ONE would have bought it. Just look at this Google trends analysis for the term “adrenal fatigue” versus “HPA axis”.
While we’re not master marketers trying to manipulate people into buying our program, we’re also not stupid. We had to use the term “adrenal fatigue” because had we not, 95% of our ideal customer base wouldn’t have even known the program was something they’d benefit from.
It’s unfortunate that the term “adrenal fatigue” is so controversial and we wish we could use the scientific term, but it’s kind of like putting toothpaste back in the tube at this point. That’s why we chose to just use the layman’s term and then educate people once they bought the program.
And I bet the term is going to stick around until medical professionals start diagnosing people with HPA Axis Dysfunction, which I doubt is going to happen anytime soon.
When it comes to Paleo Rehab: Adrenal Fatigue, Kelsey and I are really proud of the information and guidance we provide, and the results our students have gotten. I won’t apologize for using a controversial term if it allows me to help the people who need it.
What do YOU think about adrenal fatigue?
I’d love to hear your thoughts – do you think adrenal fatigue is real? Do you think HPA axis dysregulation is real? Have you made any diet or lifestyle changes that improved or eliminated your adrenal fatigue symptoms?
Share your story in the comments below!
This post may contain affiliate links. If you click on a link and make a purchase, I may receive a small commission.

+ show Comments
- Hide Comments
add a comment