Hormonal birth control – or “The Pill” – is touted by conventional gynecologists as a foolproof and completely safe way to prevent pregnancy, and to treat irregular cycles and other hormone-related disorders like PCOS and endometriosis.
Gynecologists are often too quick to prescribe the pill or an IUD without discussing some of the potential risks or consequences of using hormonal contraception.
The overuse of hormonal contraceptives in conventional medicine stems from its focus on treating symptoms of hormone dysfunction (such as PMS and menstrual irregularities) instead of correcting the underlying root of the dysfunction.
And the desire for “quick fixes” also drives many women to seek birth control for their horrible PMS symptoms, menstrual irregularities or to prevent pregnancy. According to the CDC, about 24% of reproductive age woman are using the Pill or an IUD.
But birth control is not a quick fix… and it does not truly regulate your cycles!
The Pill and hormonal IUDs use synthetic hormones that are similar, but not identical to your own estrogen and progesterone. These synthetic hormones turn off ovulation and prevent the synthesis of your own progesterone and estrogen.
Our natural estrogen and progesterone play critical roles in how we think and feel. They also drive our libido and metabolism. Synthetic hormones found in hormonal birth control fail to produce the same effect on our mood, metabolism, and libido.
As a result, many women experience negative side effects when they take the Pill. When you are considering what birth control method to use or how to balance your hormones, you need to weigh the risks and the benefits of using the Pill.
Hormonal birth control is also not the only way to prevent pregnancy. It also does nothing to promote hormonal balance as it is often believed.
I’m not saying that NO ONE should use hormonal birth control. There are situations when these hormones are entirely necessary for a woman to live a normal life. The pill may be necessary to treat debilitating endometriosis or very heavy periods that lead to anemia.
However, more often than not, doctors are prescribing hormonal birth control without educating their patients about the risks. Often times the birth control pill was never necessary to solve the problem it was prescribed for. And in many cases, the benefits don’t outweigh the risks.
Ready to take a deep dive into the possible drawbacks of hormonal birth control, and what you might do instead? Let’s go!

7 Risks of Hormonal Birth Control
1. Nutrient Depletion
Hormonal birth control can have a profound effect on nutrient status. The Pill has been shown to deplete vitamin B6, zinc, selenium, phosphorous and magnesium.
B6 and magnesium have positive effects on hormones and have been shown to relieve PMS symptoms. These nutrients are essential for the synthesis of progesterone and detoxification of estrogens. B6 also helps reduce histamine levels, which are often associated with PMS.
Ironically, many women go on the Pill for bad periods and irregular cycles that may be caused by a deficiency in magnesium or vitamin B6 only to have the Pill deplete these nutrients even further!
In addition, the Pill can lead to elevations in copper, calcium, and iron. High copper levels can lead to feelings of overstimulation, anxiety, and irritability. Iron is a pro-oxidant (opposite of an anti-oxidant), which can lead to higher levels of oxidative stress and inflammation. High calcium levels in the blood can lead to increased calcification of soft tissues like the arteries, which contributes to heart disease.
Getting adequate vitamins and minerals in your diet can be difficult and the Pill can complicate that task even further.

2. inflammation, oxidative stress, and insulin resistance
In a past Ancestral RDs podcast, hormone expert and naturopath, Dr. Jolene Brighten stated, “I run inflammatory panels [on my patients]. Everybody on the Pill is inflamed.” The scientific research also supports that the Pill is associated with increased markers of inflammation.
Oral contraceptives have been shown to raise levels of CRP (C-Reactive Protein), which is a marker of inflammation in the body. Woman taking the Pill also had higher levels of lipid peroxidation, a marker of oxidative stress. Supplemental antioxidants, vitamin C and E, improved the lipid peroxidation markers in women taking the Pill.
Dr. Brighten also pointed out in the above podcast that, “the pill skews the microbiome and creates intestinal inflammation.” This inflammation can lead to intestinal permeability (leaky gut) and systemic inflammation. The changes in the estrobolome due to the Pill could also lead to an inability to properly detox estrogens.
Nutrient deficiency and excess caused by birth control could also lead to higher levels of inflammation especially iron, which is a pro-oxidant.
Systemic inflammation caused by birth control can promote insulin resistance, which can lead to fatigue, weight gain and other more serious chronic diseases like diabetes.
3. ReduceD Thyroid Hormones
Hormonal birth control has been shown to cause low thyroid hormones by two main mechanisms. First, the Pill increases levels of thyroid hormone binding globulin.
For thyroid hormones to be used by cells, they must be free and not bound to thyroid hormone binding globulin. When oral contraceptives raise this protein, there are fewer free thyroid hormones to be used by the cells.
Second, inflammation, especially in the gut, causes a reduction in the conversion of the inactive thyroid hormone (T4) into the active hormone (T3). Without this conversion, thyroid hormones can’t exert their biological action on their target cells.
Low thyroid hormones due to hormonal birth control can lead to symptoms like fatigue, bloating, hair loss, weight gain, dry skin, and depression.

4. Depression and Mood Disturbances
Many ladies seek out birth control to help control their premenstrual irritability and moodiness. While severe mood changes prior to your cycle are not normal, the Pill or hormonal IUDs will not solve the underlying hormonal imbalance that is contributing to your mood changes.
In fact, hormonal birth control could exacerbate mood changes and contribute to depression. Mood changes are often a big reason why woman ditch the Pill.
As I mentioned before, our own estrogen and progesterone effect mood in a different way than the synthetic hormones since they are not identical. While progesterone has positive effects on brain health and cognition, its synthetic equivalent, drospirenone, is associated with depression.
A major study published in JAMA Psychiatry in 2016 revealed an increased risk of depression in women using hormonal birth control. The risk varied in severity based on the form of hormonal birth control. Compared to non-users:
- Combined birth control pill users had a 23% increase in being prescribed an anti-depressant
- Progestin-only pill users had a 34% increase in being prescribed an antidepressant
- Risks of other methods were even higher. Antidepressant prescriptions were 40% higher in those using progestin-only IUD, 60% higher for those using the vaginal ring and 100% for those using the patch
Birth controls the promotion of inflammation, oxidative stress, nutrient depletion, and thyroid suppression can all lead to feeling moody, flat, and depressed.

5. Low libido, sexual dysfunction, and infertility
It’s a bit ironic that many women go on the Pill or get an IUD so they can have sex without the fear of pregnancy, but then have no desire to have sex once they are on the pill.
Hormonal birth control has been shown to raise levels of sex hormone binding globulin. Similar to thyroid hormone binding globulin discussed above, SHBG can bind to sex hormones preventing them from exerting their effects on their target cells.
SHBG has a high affinity for testosterone. By binding to testosterone, SHBG lowers the free testosterone that can be used by your cells. This reduction in free testosterone is the primary reason why libido is often lower when on the pill. Higher levels of SHBG can also lead to estrogen dominance.
In addition to lower libido, women on the Pill are 25% more likely to experience vaginal dryness making sex a much less pleasurable experience.
SHBG has been shown to remain elevated long even after the Pill has been discontinued. This elevation can lead to sexual dysfunction and low libido even after the Pill has been discontinued!
The saddest and most serious effect that the hormonal birth control is the risk of infertility after its discontinuation. Post birth control amenorrhea is quite common after discontinuing the pill, especially for women who went on the pill to regulate their cycles.
In fact, it’s estimated that 3-6% of women may never see the return of their period post pill. And some studies suggest that women with a history of irregular periods are at higher risk of post-pill amenorrhea.
This inability to ovulate and become pregnant can be devastating to many women who stop hormonal birth control expecting that their fertility will be restored. (After all, the pill was supposed to solve their irregular or missing cycles, right?)
Would you like to save this post?
Your email address is 100% safe and will never be sent spam.
Experiencing amenorrhea, infertility and other symptoms of hormone dysfunction following discontinuation of the Pill has been termed “Post Birth Control Syndrome”.
It can be an uphill battle to repair some of the inflammatory and nutritional issues that were caused while on the Pill. Working with a skilled practitioner to repair hormone dysfunction and fertility following the Pill may be necessary.

6. Post Birth Control Acne
Birth control is often used as a treatment for hormone-related acne. The synthetic estrogens in hormonal birth control pills can dry up skin oils and acne. This effect can keep the acne at bay when you are on the Pill.
But, once you get off the Pill, the acne flood gates will open and can leave you with horrible estrogen withdrawal breakouts! These breakouts will usually fade after being off the pill for 3-4 months, but this can be a brutal process for your skin.
If you go on the Pill to help with your acne, there is a good chance that your acne may be even worse when you stop the Pill. You are much better off resolving the hormonal disturbance that is causing the acne than to go on the Pill, which will only temporarily keep the acne at bay.
7. Risk of blood clots
Blood clots are the most serious risk associated with hormonal birth control because they can be fatal.
Newer progestins found in some pills like Yaz and Yasmin have the highest risk of blood clots. A woman using Yaz has a 1.5-3 times higher chance of developing a blood clot compared to other hormonal birth control pills.
While clots are rare, it is best to rule out any family history of clotting and ask your doctor to run clotting related labs before starting any hormonal contraceptives.

Avoiding side effects of the pill
What if you and your doctor decide that hormonal birth control is the best option? Can you mitigate any potential side effects?
There’s a time and place for hormonal birth control. With severe cases of endometriosis and very heavy periods, birth control may be the best option. In these cases, there are ways to mitigate the potential side effects of the hormonal methods. These include:
- Increase intake or supplement nutrients that may be depleted by hormonal contraceptives. These include magnesium, zinc, selenium, vitamin B6 and phosphorus. In addition, you may want to monitor and track your calcium, iron and copper levels.
- Increase intake of antioxidants like vitamin C, vitamin E, and polyphenols to reduce lipid peroxidation, oxidative stress, and inflammation that can be caused by hormonal birth control.
- Consume probiotics and prebiotics to keep the gut healthy to ensure proper estrogen metabolism. Keeping your gut healthy will prevent estrogen dominance and reduce inflammation in the GI tract.
- Regular, moderate exercise to increase insulin sensitivity and prevent weight gain. (Just be careful about overdoing the exercise)
- Monitor hormone levels over time, especially thyroid and testosterone levels since the Pill can reduce free levels of these hormones. The DUTCH Plus test is my favorite way to assess hormone levels.
Is the Copper IUD a good alternative?
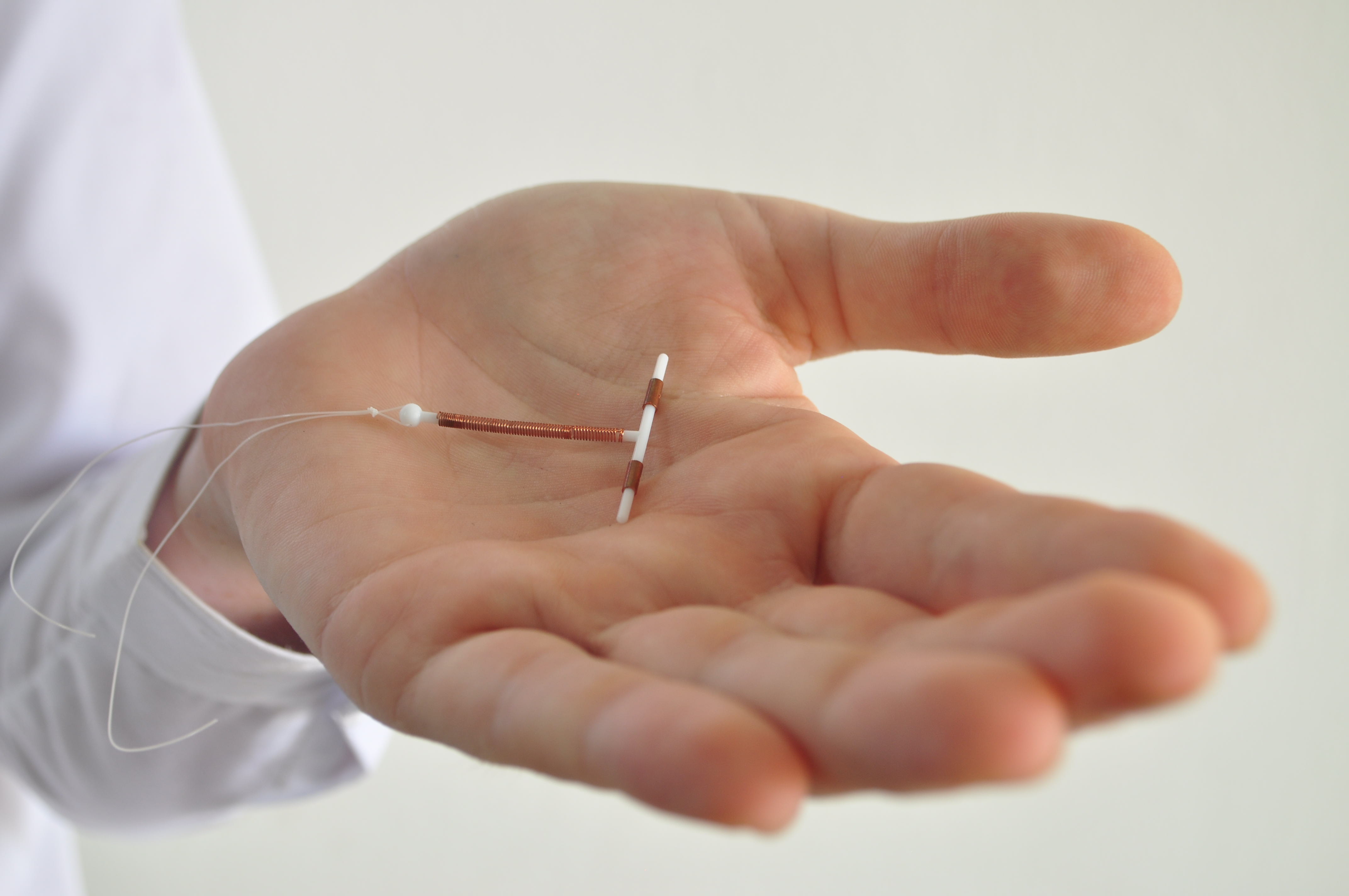
The Copper IUD often referred to by its brand name ParaGard is a non-hormonal IUD that is placed by a doctor into your uterus, and can prevent pregnancy for up to 10 years.
Unlike popular hormonal IUDs, the copper IUD does not disrupt hormone balance or ovulation. Instead, the device causes an immune response that creates a hostile environment for sperm, thereby preventing fertilization of an ovum. In addition, it appears that the device also disrupts the formation of fertilizable ova.
Dr. Lara Briden, a hormone expert and naturopath, has an awesome article about the pros and cons of copper IUDs. Here are the highlights:
The Pros of the Copper IUD include:
- The best benefit for the copper IUD is that is doesn’t disrupt ovulation like hormonal birth control methods, which stop ovulation to prevent pregnancy.
- The copper IUD has the highest user rating of any contraceptive medication on the market scoring an 8.9 out of 10 by users. This high satisfaction is probably due to the absence of synthetic hormones that often cause more symptoms and dysfunction.
- It is highly effective at preventing pregnancy with only a 0.6% failure rate.
The Cons of the Copper IUD include:
- It could cause copper toxicity, but this is very rare. The amount of copper released from the IUD is less than the copper we obtain from food. According to hormone expert Lara Briden, this slight increase only really becomes an issue if you are deficient in zinc. It is a good idea to check your zinc status and correct deficiency before insertion, and potentially supplement with zinc while you have the copper IUD in place.
- IUDs can be painful to insert and cause more cramping than hormonal birth control methods.
- You may experience heavier periods, especially in the first year.
- It may also come out leaving you at risk for pregnancy.
- You could also increase your risk of pelvic inflammatory disease in the first month after insertion but only if you have a pre-existing sexually transmitted infection.
- There is a small risk of uterine perforation which develops in 0.1% or users. A perforation will require surgery to correct.
Like any birth control method, you need to weigh the pros and cons when considering your individual case.
Overall, for most cases, the copper IUD is a better option than hormonal birth control, because it doesn’t come with all the hormone-altering risks that the Pill and hormonal IUDs do.
However, I chose not to go with the copper IUD because I’d heard some bad experiences from clients of mine. Since I’d rather not screw up my body when I’m feeling pretty good these days, I decided to forgo an IUD altogether.

My Preferred Method of Birth Control
That being said, my preferred method of birth control is the Fertility Awareness Method or FAM!
The Fertility Awareness Method (pssst… NOT the “rhythm” method) is an effective way to predict fertile and infertile times in your cycle. FAM is based on body signs, specifically basal body temperature and cervical mucus, which change during each menstrual cycle in response to the hormones that cause ovulation.
If natural family planning is followed correctly, it can be up to 99% effective. This means that 1 woman in 100 who use natural family planning will get pregnant in 1 year. There are no physical side effects, and you can either use it as a contraceptive method or to plan when you get pregnant.
There are 3 different fertility signs you can monitor and record for more accurate fertility awareness and natural family planning. These are:
- the length of your menstrual cycle (your period starts on Day 1)
- daily readings of your basal body temperature (your temperature before getting out of bed in the morning)
- changes to your cervical secretions (cervical mucus)
You need to use a special basal body temperature thermometer that measures to the 100th decimal point to get a more accurate temperature reading (don’t use your regular old illness thermometer!)
After ovulation, each egg only lives for a maximum of 24 hours, and sperm must meet the egg within that period for pregnancy to happen. So technically you’re only fertile for about 24 hours per month. But because the sperm can survive for 5 days in optimal conditions, the true length of your fertile window is about 5-6 days total.
During your fertile window, to prevent pregnancy you’ll need to use a barrier method of contraception, such as a condom or diaphragm. (I personally like these condoms myself.) Alternatively, you can simply forgo sex during your fertile window to be absolutely certain you won’t get pregnant.
Use one of these charts to track your data, and make sure you use the FAM method for at least 3 months before you start using it as a contraceptive tool. You can use a barrier method or abstain from sex during this time while you are learning your cycles.
Here’s a great, short overview of FAM and how you can use it to prevent or achieve pregnancy.
The book Taking Charge of Your Fertility is a comprehensive overview of this method. The best part about FAM is that you learn so much about your body while you’re doing it, and there’s zero impact on your own health.
There are a few amazing things to learn in the TCOYF book, including:
- If your body isn’t producing fertile cervical mucus, the sperm will die inside you in a few hours
- If your body IS producing fertile cervical mucus, sperm can live inside you for 5 days!
- A lack of temperature shift and/or cervical fluid changes can indicate an anovulatory cycle, which is a menstrual cycle where you don’t ovulate (and thus are not fertile)
- Your fertility signals (and ovulation) can be immediately affected by illness, stress, and travel
- The length of your luteal phase (post-ovulation) can indicate low progesterone levels if it’s too short
This is definitely one of my favorite books to recommend for women to understand their bodies and to work with their hormones for optimizing their health and wellbeing every month.
Finally, I’ll admit that the charting method is a little too time consuming for me at this point in my life. I may consider tracking cervical fluid at some point but right now, I’m using a different, more convenient way to track my fertile windows.
 That method is the Daysy thermometer!
That method is the Daysy thermometer!
The Daysy is a fertility tracker that uses the fertility awareness method by learning and tracking your menstrual cycle. The thermometer also has a computer insider to keep track of your data over time.
All your data can be synced to the app on your phone so you can see how your temperature and your overall cycle is tracking over time!
Daysy tells you when you’re in your fertile window with an accuracy of 99.4%. Your fertility status will be displayed either as a red (fertile) or green (not fertile) light. Simply use a barrier method during the days that you see a red light and you’re good to go!
Keep in mind, the Daysy monitor, and FAM in general, can’t be used for contraception in women with very irregular cycles. The Daysy can safely recognize cycles that range between 19 and 40 days. However, using Daysy with extreme fluctuations would lead to a higher number of red/yellow days.
And if your cycles are regularly beyond 40 days, you should be using a barrier method to prevent pregnancy while you’re working with a trained practitioner to figure out why your cycles are so long.
Now I want to hear from you… what’s your preferred method of birth control? Have you had a good or bad experience with an IUD? Share your story in the comments below!
This post may contain affiliate links. If you click on a link and make a purchase, I may receive a small commission.

+ show Comments
- Hide Comments
add a comment